Monday, 27 January 2014
Sunday, 19 January 2014
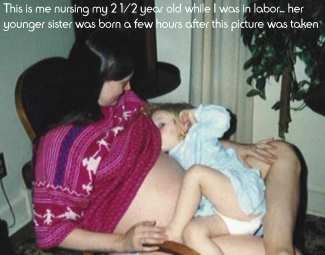
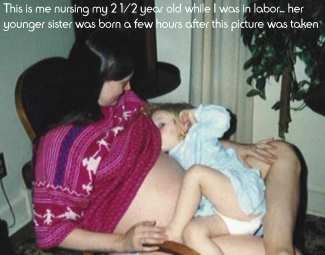
Tandem Nursing
An Article on Tandem Nursing by Anna Smith (IBCLC).
The AAP (American Academy of Pediatrics) recommends exclusively breastfeeding your baby for the first six months of life, with no solids or supplements, and continuing to nurse throughout the first year of life and beyond. During the period of exclusive breastfeeding, it is very unlikely that you will become pregnant. However, as more and more mothers recognize the advantages of long-term nursing and natural weaning, more of them will become pregnant while they are nursing their baby.
The mother facing the decision of whether to wean or continue nursing during her pregnancy often has mixed emotions, and may get conflicting advice from friends, family, and health care providers. The most common concern is whether continuing to breastfeed will put the expected baby at risk in some way. There is no evidence to suggest that nursing while pregnant endangers the fetus during a normal pregnancy. If a mother has previously delivered a premature baby, develops signs of pre-term labor, or is carrying multiples, there is concern that a hormone released during lactation (oxytocin) may stimulate contractions and trigger a premature labor. In these special situations, mothers are often advised to wean their older child. Research suggests that the uterus is not receptive to hormonal stimulation from oxytocin until around 24 weeks gestation, so it is generally safe to consider nursing until about 20 weeks, even in these special situations. There is almost never a need to wean abruptly during pregnancy.
The mother who is deciding whether to continue nursing during her pregnancy has several factors to consider: her medical history, her physical and emotional comfort level, the nursing child’s age, and his need to nurse. If the pregnancy is progressing normally, then the decision of whether to continue to breastfeed is more an individual ‘parenting’ decision rather than a ‘medical’ decision.

There is no evidence that nursing during a pregnancy will cause miscarriage during the early months. Miscarriage occurs spontaneously in about 16-30 percent of all pregnancies, so it will sometimes happen while a mother is nursing. The nursing mother should not add the burden of guilt to the pain of losing a baby to miscarriage.
Nursing during pregnancy will not deprive the fetus of essential nutrients, and will not create a harmful “drain” on the mother’s body. During pregnancy, it is always important to eat nutritiously, gain weight appropriately, and get adequate rest. A well-nourished mother should have no problem providing enough nutrients for both her unborn baby and her nursing child.
Breastfeeding provides several opportunities each day for the expectant mother to take breaks and rest while her toddler nurses or naps.
Due to hormonal changes, most mothers will experience some degree of nipple soreness during pregnancy, which can make nursing very uncomfortable. Nipple soreness is the most common reason given for weaning during pregnancy. The soreness usually is most pronounced during the early months of pregnancy. Since the cause of the soreness is hormonal, there is no real treatment other than time. Some mothers find relief by reducing the time the baby spends at the breast, limiting nursing sessions to nap and bed-time,and others find that reminding the toddler to “open wide” while latching on may reduce soreness.
During pregnancy, most mother’s milk supply will decrease due to hormonal changes. During the second trimester, the milk will begin to change to colostrum. Both the quantity and the taste of the milk change dramatically during this time, and many babies will wean themselves when the milk changes. If you are nursing a baby younger than 6 months when you become pregnant, you will need to carefully monitor his growth and weight gain, and supplemental feedings may be necessary. Older babies who are eating solids will usually show an increased appetite for other foods as your milk supply decreases.
Some babies don’t seem to care whether they are getting a lot of milk when they nurse. That’s where the emotional component of breastfeeding becomes a factor. Babies vary in their need for oral satisfaction, physical contact, closeness to mother, and willingness to have those needs met in ways other than nursing.
Some toddlers continue to find breastfeeding very important all the way through the pregnancy and after the birth of the new baby as well. Nursing siblings who are not twins is called “tandem nursing”. In our culture, this concept is unusual, although other in many other cultures it is a common practice. It is not unusual to have mixed feelings about nursing during pregnancy or tandem nursing. Negative feelings are common, due to physical discomfort and fatigue, as well as feeling “touched out” after nursing for so many months. For the mother who finds herself resenting the older baby’s demands, and has difficulty focusing enough attention on the new baby, weaning may be the best choice. She should try to wean gradually, nursing the new baby when the toddler is occupied with other things, and substituting special activities and snacks for nursings. Dads can be a big help with this process.
When they choose to tandem nurse, many mothers find that a unique closeness develops between their nursing siblings. Sharing at the breast can reduce the jealously and sibling rivalry that often accompanies the arrival of a new baby.
Because the older child is receiving nourishment from foods other than breastmilk, the newborn should be allowed to nurse first, ensuring that he gets lots of colostrum. Nursing a toddler can help relieve engorgement. Because the toddler will nurse more vigorously than the infant, the mother may find that she produces an oversupply of milk. If this occurs, and the newborn chokes when attempting to nurse, she may want to let the toddler nurse briefly before putting the new baby on the breast. Within a short period of time, the milk supply will adjust to the needs of the two siblings, just as it would if the mother were nursing twins or triplets. The two nurslings can be fed at the same time, or separately – whatever works best for you.
The mother facing the decision of whether to wean or continue nursing during her pregnancy often has mixed emotions, and may get conflicting advice from friends, family, and health care providers. The most common concern is whether continuing to breastfeed will put the expected baby at risk in some way. There is no evidence to suggest that nursing while pregnant endangers the fetus during a normal pregnancy. If a mother has previously delivered a premature baby, develops signs of pre-term labor, or is carrying multiples, there is concern that a hormone released during lactation (oxytocin) may stimulate contractions and trigger a premature labor. In these special situations, mothers are often advised to wean their older child. Research suggests that the uterus is not receptive to hormonal stimulation from oxytocin until around 24 weeks gestation, so it is generally safe to consider nursing until about 20 weeks, even in these special situations. There is almost never a need to wean abruptly during pregnancy.
The mother who is deciding whether to continue nursing during her pregnancy has several factors to consider: her medical history, her physical and emotional comfort level, the nursing child’s age, and his need to nurse. If the pregnancy is progressing normally, then the decision of whether to continue to breastfeed is more an individual ‘parenting’ decision rather than a ‘medical’ decision.

Nursing during pregnancy will not deprive the fetus of essential nutrients, and will not create a harmful “drain” on the mother’s body. During pregnancy, it is always important to eat nutritiously, gain weight appropriately, and get adequate rest. A well-nourished mother should have no problem providing enough nutrients for both her unborn baby and her nursing child.
Breastfeeding provides several opportunities each day for the expectant mother to take breaks and rest while her toddler nurses or naps.
Due to hormonal changes, most mothers will experience some degree of nipple soreness during pregnancy, which can make nursing very uncomfortable. Nipple soreness is the most common reason given for weaning during pregnancy. The soreness usually is most pronounced during the early months of pregnancy. Since the cause of the soreness is hormonal, there is no real treatment other than time. Some mothers find relief by reducing the time the baby spends at the breast, limiting nursing sessions to nap and bed-time,and others find that reminding the toddler to “open wide” while latching on may reduce soreness.
During pregnancy, most mother’s milk supply will decrease due to hormonal changes. During the second trimester, the milk will begin to change to colostrum. Both the quantity and the taste of the milk change dramatically during this time, and many babies will wean themselves when the milk changes. If you are nursing a baby younger than 6 months when you become pregnant, you will need to carefully monitor his growth and weight gain, and supplemental feedings may be necessary. Older babies who are eating solids will usually show an increased appetite for other foods as your milk supply decreases.
Some babies don’t seem to care whether they are getting a lot of milk when they nurse. That’s where the emotional component of breastfeeding becomes a factor. Babies vary in their need for oral satisfaction, physical contact, closeness to mother, and willingness to have those needs met in ways other than nursing.
Some toddlers continue to find breastfeeding very important all the way through the pregnancy and after the birth of the new baby as well. Nursing siblings who are not twins is called “tandem nursing”. In our culture, this concept is unusual, although other in many other cultures it is a common practice. It is not unusual to have mixed feelings about nursing during pregnancy or tandem nursing. Negative feelings are common, due to physical discomfort and fatigue, as well as feeling “touched out” after nursing for so many months. For the mother who finds herself resenting the older baby’s demands, and has difficulty focusing enough attention on the new baby, weaning may be the best choice. She should try to wean gradually, nursing the new baby when the toddler is occupied with other things, and substituting special activities and snacks for nursings. Dads can be a big help with this process.
When they choose to tandem nurse, many mothers find that a unique closeness develops between their nursing siblings. Sharing at the breast can reduce the jealously and sibling rivalry that often accompanies the arrival of a new baby.
Because the older child is receiving nourishment from foods other than breastmilk, the newborn should be allowed to nurse first, ensuring that he gets lots of colostrum. Nursing a toddler can help relieve engorgement. Because the toddler will nurse more vigorously than the infant, the mother may find that she produces an oversupply of milk. If this occurs, and the newborn chokes when attempting to nurse, she may want to let the toddler nurse briefly before putting the new baby on the breast. Within a short period of time, the milk supply will adjust to the needs of the two siblings, just as it would if the mother were nursing twins or triplets. The two nurslings can be fed at the same time, or separately – whatever works best for you.
There are no special concerns about hygiene. The nipple secretes an enzyme that reduces bacterial counts, and breastfed babies are born with immunities to most germs found in their home environment. Most germs involved in common illnesses are contagious for days before symptoms appear, so tandem nursers have been exposed by the time you know one of them is ill. If you are dealing with a serious illness, one that is very contagious, or thrush, you may want to limit each child to one breast temporarily.
Sometimes a toddler who was weaned before the new baby’s arrival will decide that he wants to nurse again. Often a discussion of how he used to nurse, but now he’s a “big boy” and can eat grown up food, will suffice. If he is insistent about it, it is probably best to let him try. Most of the time toddlers who have weaned have forgotten how to nurse, and will lose interest quickly. Allowing him to nurse until he feels more secure about his new position in the family can be a good idea.
Tandem nursing is not for everyone. If it is not working out well, mothers should wean the older child without feeling guilty about it. It is important to give the older baby lots of extra cuddling and attention so that he knows that although he is losing the comfort and security of the breast, he is not losing his mother’s love.
If a mother does choose to tandem nurse, she can find it very gratifying for everyone involved. Knowing that she nursed her baby until he outgrew the need is a very rewarding feeling, and can result in increased security and self-esteem in the child who weans when he is ready to move on to the next stage of his development, and not just because his mother became pregnant.
(Edited October, 2013)
Anne Smith, IBCLC
Saturday, 11 January 2014
Fenugreek (as Milk Booster) During Pregnancy
Hi Mummies!
Recently I was approached by a Mummy who is Breastfeeding her 1 year and 3 months old child. She is also Pregnant with her second child (7 weeks POG).
She asked was it safe to take Fenugreek (As Milk Booster) during Pregnancy?
 |
| Fenugreek Seeds |
Probably this few sentences from few resources would help summarize the answer:
"Fenugreek is LIKELY UNSAFE in pregnancy when used in amounts greater than those in food. It might cause early contractions. Taking fenugreek just before delivery may cause the newborn to have an unusual body odor, which could be confused with “maple syrup disease.” It does not appear to cause long-term effects."
Source: http://www.webmd.com/vitamins-supplements/ingredientmono-733-FENUGREEK.aspx?activeIngredientId=733&activeIngredientName=FENUGREEK
"Avoid use in pregnancy as fenugreek has documented uterine stimulant effects. It has been used to stimulate milk production in nursing mothers. Excretion into milk has not been studied."
Source: http://www.drugs.com/npc/fenugreek.html
"Traditionally, fenugreek has been used to stimulate labor. However, this does not mean that it is safe or effective for such use, since it has never been studied for such purposes. For instance, think about the many strange ways women try to induce labor (such as eating kiwi, eating spicy foods, or taking bumpy car rides). There is no real way to know if these methods are effective, even if they work. It could very easily just be coincidence.
Even though there is no research to suggest that fenugreek works for stimulating labor, it is a good idea to avoid taking it unless you are full-term (37 weeks pregnant or beyond). If fenugreek does happen to be effective for stimulating uterine contractions, which is currently unknown, it could cause preterm labor or miscarriages if taken earlier in pregnancy. Also, there have been reports of body or urine odor smelling like maple syrup in infants after fenugreek was used for labor stimulation (the herb contains a compound that smells like maple syrup). Sometimes, this is mistaken by medical providers as a rare but serious condition known as maple syrup disease.
Pregnancy is not a time to be experimenting with herbs or medications. It is best to stick with products that are known to be safe for pregnant women. As an herb that has been studied very little, fenugreek is not one of these products."
Note: The above are merely paragraphs taken from different resources. To read whole article, mummies may click on the links above.
Moral of The Story, Do Consult you Healthcare Proffesional before starting any Herbs/Supplements/Medications during Breastfeeding and Pregnancy :-)
Much LOVE <3
Tuesday, 7 January 2014
Breastfeeding May Prevent Arthritis: New Study
Tuesday, 17 December 2013
Senarai Semak Untuk Ibu Bekerja
Lampiran di bawah ini adalah khas buat Ibu-Ibu tersayang yang ingin menyusukan anak dengan Penyusuan Susu Ibu walaupun sibuk bekerja. Adakah Ibu-Ibu sudah sedia? :-)
Lampiran ini adalah petikan dari Buku "Panduan Lengkap Bagi Ibu & Wanita Bekerjaya" terbitan Persatuan Penyokong-Penyokong Penyusuan Ibu & Bayi Malaysia.
Semoga berjaya Menyusukan Anak-anak dengan Susu Ibu! :-)
Semoga berjaya Menyusukan Anak-anak dengan Susu Ibu! :-)
Monday, 16 December 2013
Breastfeeding Keeps Mummies Slim :-)
The article below is abstracted from www.dailymail.co.uk. Published on 10th of July 2012.
Original article titled :
Breastfeeding your baby for six months will 'keep you slim in later life'
Many mothers have long believed that breastfeeding helps them to get their figure back after giving birth.Now scientists have found it can help them to stay slim for decades.
They discovered that women who breastfed their babies even for a few months after the birth were less likely to be obese 30 years later.

The Oxford University researchers worked out that for every six months a woman gives her baby breast milk, she loses around 2lb – depending on her initial weight and height.
Although this may not sound much, the academics claim that it could help prevent thousands of deaths from cancer, heart problems and other illnesses related to obesity.
Doctors and midwives are growing increasingly concerned that many women are becoming obese by gaining weight during pregnancy, which they never manage to shift after the birth.
The latest study – involving more than 740,000 women – provides compelling evidence that breastfeeding could help reverse this weight gain, and then help women keep the weight off for good.
Breastfeeding uses up large amounts of energy and experts have previously calculated it burns 500 calories a day – the same as a typical gym session.
Now academics have worked out that for every six months a woman breastfeeds her baby, her body mass index – the measurement of obesity – falls by 1 per cent. An average woman who is 5ft 6ins tall and weighs 11st 1lb would have a BMI measurement of 25, which is classified as overweight.
 But if her BMI was to fall by 1 per cent it would be about 24.75 – which is deemed ‘healthy’ – and she would weigh 10st 13lb.
But if her BMI was to fall by 1 per cent it would be about 24.75 – which is deemed ‘healthy’ – and she would weigh 10st 13lb.
The lead author of the paper, Dr Kirsty Bobrow, from Oxford University, said: ‘We already know breastfeeding is best for babies, and this study adds to a growing body of evidence that the benefits extend to the mother as well – even 30 years after she’s given birth.
Although this may not sound much, the academics claim that it could help prevent thousands of deaths from cancer, heart problems and other illnesses related to obesity.
Doctors and midwives are growing increasingly concerned that many women are becoming obese by gaining weight during pregnancy, which they never manage to shift after the birth.
Oxford University researchers worked out that for every six months a woman gives her baby breast milk, she loses around 2lb – depending on her initial weight and height.
If they go on to have several children, they will become progressively fatter with every pregnancy.The latest study – involving more than 740,000 women – provides compelling evidence that breastfeeding could help reverse this weight gain, and then help women keep the weight off for good.
Breastfeeding uses up large amounts of energy and experts have previously calculated it burns 500 calories a day – the same as a typical gym session.
Now academics have worked out that for every six months a woman breastfeeds her baby, her body mass index – the measurement of obesity – falls by 1 per cent. An average woman who is 5ft 6ins tall and weighs 11st 1lb would have a BMI measurement of 25, which is classified as overweight.

The lead author of the paper, Dr Kirsty Bobrow, from Oxford University, said: ‘We already know breastfeeding is best for babies, and this study adds to a growing body of evidence that the benefits extend to the mother as well – even 30 years after she’s given birth.
‘Pregnant women should be made aware of these benefits to help them make an informed choice about infant feeding.’ The researchers also point out that breastfeeding may help prevent thousands of deaths related to obesity from cancer, heart disease and diabetes.
Professor Dame Valerie Beral, director of the Cancer Epidemiology Unit at Oxford University, who was also involved in the study, said: ‘Our research suggests that just six months of breastfeeding by UK women could reduce their risk of obesity in later life.
‘A 1 per cent reduction in BMI may seem small, but spread across the population of the UK that could mean about 10,000 fewer premature deaths per decade from obesity-related conditions, such as diabetes, heart disease and some cancers.’
The study, published in the International Journal of Obesity, surveyed 740,600 women whose average age was 57. They had all answered questions about how many children they had and the total number of months they had spent breastfeeding.
The research also found that women were more likely to be obese if they had several children.
This backs up the concerns of health professionals that many gain weight during pregnancy which they don’t lose after the birth of their babies.
According to the latest figures from the Department of Health, almost three quarters of new mothers start their babies off on breast milk.
This is far higher than the six in ten who breastfed in the 1990s and the rise follows numerous ‘breast is best’ campaigns.
The World Health Organisation recommends that women breastfeed their babies for at least six months but many give up because they find it uncomfortable or are worried that their babies are struggling to get enough milk.
Thursday, 12 December 2013
Tips for NURSING IN PUBLIC
Breastfeeding mothers and their babies shouldn’t feel they have to stay home.
They want to enjoy the same activities as anyone else! Current Malaysian Breastfeeding Policy is to breastfeed exclusively for six months and to continue breastfeeding with added complementary foods for two years and beyond.
Many mothers are already perfectly comfortable breastfeeding in public. That’s great – not only for you and your baby, but for those women and girls who are not yet mothers, who learn about breastfeeding when they see you.
But maybe that’s not you. Maybe you are feeling pretty anxious about nursing in public. You worry about what people will think, and how much skin you’ll be showing. These tips may help:
1. Know your rights. Breastfeeding in public is legal and a very good thing. You are nourishing your baby with the most biologically appropriate food, and – as a great side benefit – you are educating any young men and women who might happen to see you. The Ontario Human Rights Commission, for instance, specifically states:
No one should prevent you from nursing your child simply because you are in a public area. They should not ask you to “cover up,” disturb you, or ask you to move to another area that is more “discreet.”
2. Practise at home in front of a mirror. If you’ve been concerned about showing a lot of skin, this will probably reassure you that it’s not likely to be an issue. A nursing baby covers your breast rather efficiently. You can try nursing in different outfits to see which ones work for you and your baby. Some babies can’t stand any fabric touching their faces as they nurse, others are less bothered by it, so experiment to find your best options.
3. Choose clothes you’ll feel comfortable in. You can buy (or sew) specially-made nursing clothes that have hidden openings to make breastfeeding easier, or you can put together nursing outfits from ordinary clothes.
4. Use a sling or wrap. With practice, you can breastfeed your baby in most slings or wrap and the fabric of the baby carrier will cover the baby and your breast. You can even walk around while breastfeeding!
5. Use a Nursing Cover. Specially made nursing Poncho; baby blankets; long & wide shawls or lengthy head-cover (tudung-for Muslim Mummies) can be useful to maintain modesty while nursing in public.
 |
| Beautiful Mummy Nursing in Public using Eve Love Nursing Poncho |
5. Choose an easy-access bra. If you are using a nursing bra where you need to lower the cup, it might help to practise undoing it one-handed at home (and doing it up again after) so that you’re confident about managing it out in public.
6. Pick your spot. You’re looking for two things: a place where you can sit comfortably, ideally with some support for your back, as well as a place where you are less visible to the general public. In a restaurant, sitting towards the inside of a booth means you’ll mainly be seen by your dining companions; if there are no booths you can pick a seat at a table facing away from the dining room. Outdoors, you may be able to find a place to sit leaning against a tree or a bench with a back that gives you support.
Don’t get stressed out looking for the perfect spot. Find a place where you’re comfortable and where you have enough room to organize yourself and don’t worry too much about who might see you. There’s no point in walking around with a crying baby as you look for a place where you won’t be visible. Feeding your child takes priority.
7. Turn away to latch. The time when the most skin is likely to be shown is when the baby is first latching on. So let’s say you are sitting in a restaurant booth, next to the wall, but still visible to other diners. Before you latch the baby on, try turning so you are completely facing the wall. Latch your baby on in this position, then turn back to face the table and your dining companions. You can do the same if you need to unlatch the baby.
8. Smile! If you notice someone glancing in your direction as you breastfeed your baby, even if they are frowning or looking horrified, give them a smile! You know you are doing something very important for your child, and that’s a good thing. If you show your confidence with a friendly smile, you may defuse the situation.
Subscribe to:
Posts (Atom)