Breastfeeding Myths
To mothers out there, breastfeeding or not, it is my obligation to spread the word of truth on breastfeeding so that you get a clear picture with regards to breastfeeding. Words of myth are spread throughout, in every community, every region and every country. The latest and funniest I’ve heard by far is from a friend who claimed that her grandmother told her this:
‘ Whenever you breastfeed your baby, feed the right breast first, then the left. This is because the milk from the right breast represents rice and the milk from the left breast represents water’.
Such statement might not make sense for mothers who are well-educated on breastfeeding but might affect the mind of some young mothers who are ignorant on breastfeeding, hence giving them unnecessary pressure to make sure they synchronize the feeding according to the proper order of which breast to feed first.
I would love to share a few famous breastfeeding myths in relation to Dr. Jack Newman’s article on Breastfeeding Myths.
1. Many women do not produce enough milk.
Not true! The vast majority of women produce more than enough milk. The usual reason that the baby does not get the milk that is available is that he is poorly latched onto the breast. This is why it is so important that the mother be shown, on the first day, how to latch a baby on properly, by someone who knows what they are doing.
2. It is normal for breastfeeding to hurt.
Not true! Though some tenderness during the first few days is relatively common, this should be a temporary situation which lasts only a few days and should never be so bad that the mother dreads nursing. Causes of breast or nipple pain include poor baby latching, yeast infection, plugged ducts and many others. Please consult a physician if you experience prolong breast or nipple pain.
3. There is no (not enough) milk during the first 3 or 4 days after birth.
Not true! It often seems like that because the baby is not latched on properly and therefore is unable to get the milk. Once the mother's milk is abundant, a baby can latch on poorly and still may get plenty of milk. By not latching on well, the baby is unable to get the mother's first milk, called colostrum. Anyone who suggests you pump your milk to know how much colostrum there is, does not understand breastfeeding, and should be politely ignored.
4. A baby should be on the each side of the breast for a certain amount of time.
Not true! A distinction needs to be made between "being on the breast" and "breastfeeding". If a baby has latched on properly and drank sufficiently on the first breast, it is not necessary for he/she might to drink from the other side.
5. A breastfeeding baby needs extra water in hot weather.
Not true! Breastmilk contains all the water a baby needs.
6. A mother should wash her nipples each time before feeding the baby.
Not true! Formula feeding requires careful attention to cleanliness because formula not only does not protect the baby against infection, but also is actually a good breeding ground for bacteria and can also be easily contaminated. On the other hand, breastmilk protects the baby against infection. Washing nipples before each feeding makes breastfeeding unnecessarily complicated and washes away protective oils from the nipple.
7. Pumping is a good way of knowing how much milk the mother has.
Not true! How much milk can be pumped depends on many factors, including the mother's stress level. Babies are the best pump!
8. Breastfeeding ties the mother down.
Not true! A baby can be nursed anywhere, anytime, and thus breastfeeding is liberating for the mother. No need to drag around bottles or formula. No need to worry about where to warm up the milk. No need to worry about sterility. No need to worry about how your baby is, because he is with you.
9. There is no way to know how much breastmilk the baby is getting.
Not true! There are ways to measure if your baby is getting enough such as urine output and colour, stool consistency, weight gain and many more.
10. Modern formulas are almost the same as breastmilk.
Not true! There is no duplicate for God’s natural gift for babies.
11. If the mother has an infection she should stop breastfeeding.
Not true! The baby's best protection against getting the infection is for the mother to continue breastfeeding. If the baby does get sick, he will be less sick if the mother continues breastfeeding. Besides, maybe it was the baby who gave the infection to the mother, but the baby did not show signs of illness because he was breastfeeding. Also, breast infections, including breast abscess, though painful, are not reasons to stop breastfeeding. Indeed, the infection is likely to settle more quickly if the mother continues breastfeeding on the affected side.
12. If the baby has diarrhea or vomiting, the mother should stop breastfeeding.
Not true! The best medicine for a baby's gut infection is breastfeeding. Stop other foods for a short time, but continue breastfeeding. Breastmilk is the only fluid your baby requires when he has diarrhea and/or vomiting, except under exceptional circumstances. The push to use "oral rehydrating solutions" is mainly a push by the formula (and oral rehydrating solutions) manufacturers to make even more money. The baby is comforted by the breastfeeding, and the mother is comforted by the baby's breastfeeding.
13. If the mother is taking medicine she should not breastfeed.
Not true! There are very few medicines that a mother cannot take safely while breastfeeding.
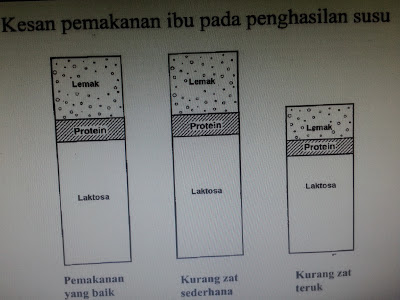
14. A breastfeeding mother has to be obsessive about what she eats.
Not true! A breastfeeding mother should try to eat a balanced diet, but neither needs to eat any special foods nor avoid certain foods. A breastfeeding mother does not need to drink milk in order to make milk. A breastfeeding mother does not need to avoid spicy food.
15. A breastfeeding mother has to eat more in order to make enough milk.
Not true! It is commonly said that women need to eat 500 extra calories a day in order to breastfeed. This is not true. Some women do eat more when they breastfeed, but others do not, and some even eat less, without any harm done to the mother or baby or the milk supply. The mother should eat a balanced diet dictated by her appetite. Rules about eating just make breastfeeding unnecessarily complicated.
16. A breastfeeding mother has to drink lots of fluids.
Not true! The mother should drink according to her thirst. Some mothers feel they are thirsty all the time, but many others do not drink more than usual. The mother's body knows if she needs more fluids, and tells her by making her feel thirsty.
17. A mother who bleeds from her nipples should not breastfeed.
Not true! Though blood makes the baby spit up more, and the blood may even show up in his bowel movements, this is not a reason to stop breastfeeding the baby. The mother should breastfeed! If bleeding does not stop soon, the source of the problem needs to be investigated, but the mother should keep breastfeeding.
18. Premature babies need to learn to take bottles before they can start breastfeeding.
Not true! Premature babies are less stressed by breastfeeding than by bottle feeding. A baby as small as 1200 grams and even smaller can start at the breast as soon as he is stable, though he may not latch on for several weeks.
19. Babies with cleft lip and/or palate cannot breastfeed.
Not true! Some do very well. The baby's ability to breastfeed does not always seem to depend on the severity of the cleft. Breastfeeding should be started, as much as possible, using the principles of proper establishment of breastfeeding. If bottles are given, they will undermine the baby's ability to breastfeed. If the baby needs to be fed, but is not latching on, a cup can and should be used in preference to a bottle.
20. Women with small breasts produce less milk than those with large breasts.
Nonsense!
 |
| Breasts come in various shapes & sizes but all are made with lots of structures to produce breastmilk beneath! |
21.Breastfeeding babies need other types of milk after 6 months.
Not true! Breastmilk gives the baby everything there is in other milks and more. Babies older than 6 months should be started on solids mainly so that they learn how to eat and so that they begin to get another source of iron, which by 7-9 months, is not supplied in sufficient quantities from breastmilk alone. Thus cow's milk or formula will not be necessary as long as the baby is breastfeeding.
22. Breastfeeding mothers' milk can "dry up" just like that.
Not true! Or if this can occur, it must be a rare occurrence. Stick to the rule of `Supply vs Demand’ where you should keep on breastfeeding and pumping. The more you express or breastfeed; more milk will come.
23. Physicians and paediatricians know a lot about breastfeeding.
Not true! Obviously, there are exceptions.
24.Breastmilk given with formula may cause problems for the baby.
Not true! There is no reason that breastmilk and formula cannot be given together.
25. There is no such thing as nipple confusion.
Not true! Babies who are bottle-fed at a very young age even before they are familiar with the breast might not want to latch on mother’s breast because the flow of the artificial nipples are much faster that natural flow from the mother’s breast. Hence, the baby has to work harder to in order to drink. Cup feeding is an alternative to avoid nipple confusion.
26.Women with flat or inverted nipples cannot breastfeed.
Not true! Babies do not breastfeed on nipples, they breastfeed on the breast. Though it may be easier for a baby to latch on to a breast with a prominent nipple, it is not necessary for nipples to stick out. Breasts change in the first few weeks, and as long as the mother maintains a good milk supply, the baby will usually latch on, sooner or later.
 |
| Mummies with inverted or flat nipples can ease latching with this method |
27. A woman who becomes pregnant must stop breastfeeding.
Not true! If the mother and child desire, breastfeeding can continue. There are women who continue nursing the older child even after delivery of the new baby. Many women do decide to stop nursing when they become pregnant because their nipples are sore, or for other reasons, but there is no rush nor medical necessity to do so. In fact, there are often good reasons to continue. The milk supply may decrease during pregnancy, but if the baby is taking other foods, this is not a problem.
28. If a mother has surgery, she has to wait a day before restarting nursing.
Not true! The mother can breastfeed immediately after surgery, as soon as she is up to it. Neither the medications used during anaesthesia, nor pain medications nor antibiotics used after surgery require the mother to avoid breastfeeding, except under exceptional circumstances.
29. A mother whose breasts do not seem full has little milk in the breast.
Not true! Breasts do not have to feel full to produce plenty of milk. It is normal that a breastfeeding woman's breasts feel less full as her body adjusts to her baby's milk intake. This can happen suddenly and may occur as early as two weeks after birth or even earlier. The breast is never "empty" and also produces milk as the baby nurses.
30. Breastfeeding in public is not decent.
Not true! Mothers have all the right to provide the best for their babies anytime, anywhere.
31. If the baby is off the breast for a few days (weeks), the mother should not restart breastfeeding because the milk sours.
Not true! The milk is as good as it ever was.
33. Breastfeeding is blamed for everything.
True! The toughest obstacle of breastfeeding is the uncooperative people that you might encounter. Stay strong, for you and the baby!